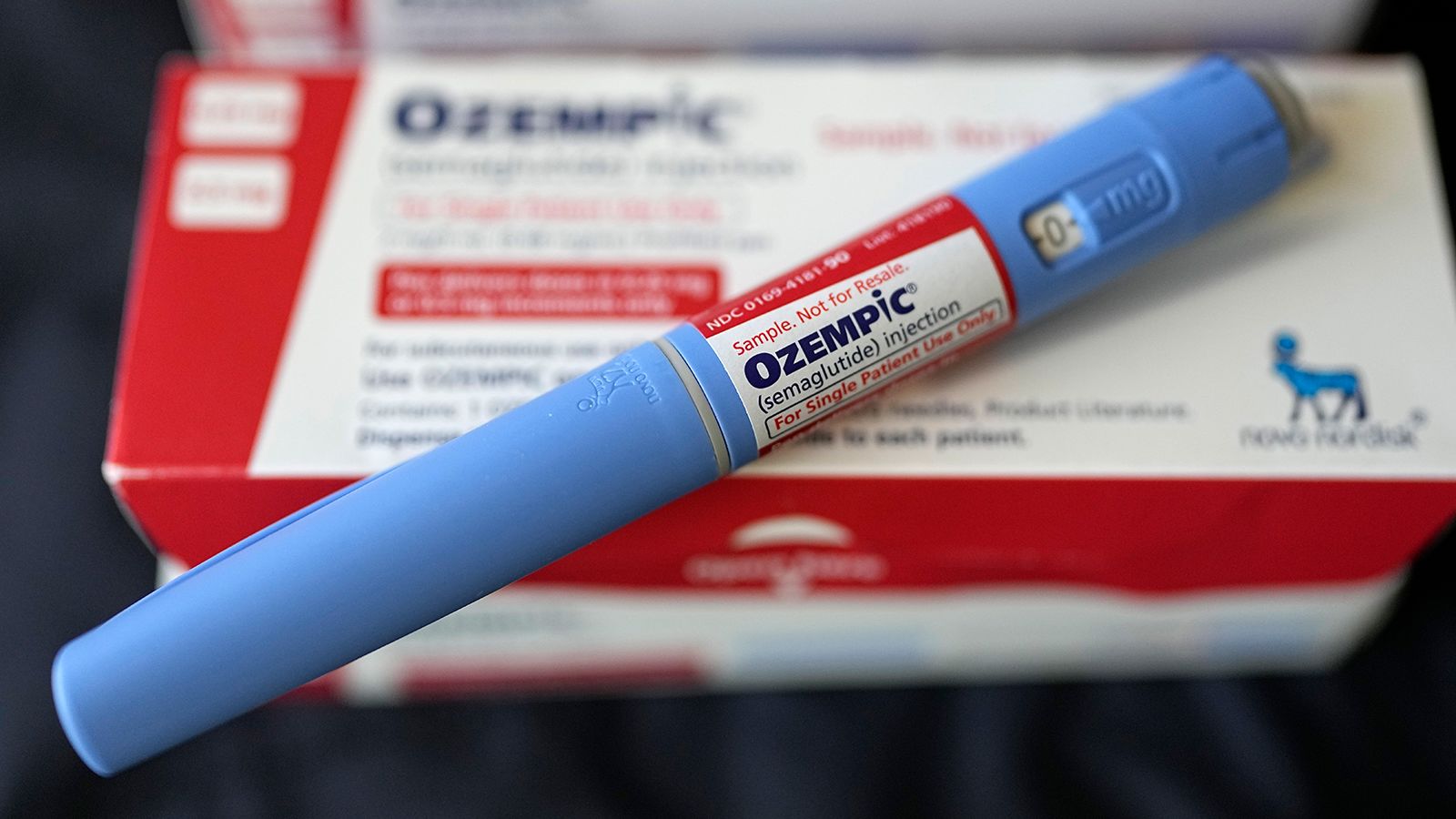
(CNN) — Some Americans may have to pay more this year for Ozempic and Monzaro, two popular diabetes drugs that are also used for weight loss.
Manufacturers raised the list prices of the two drugs, along with nearly 900 other brand-name drugs, in January, according to 46Brooklyn, a nonprofit drug pricing analysis firm.
The average increase was 4.7%, slightly below the typical annual increase since 2019 and much lower than the roughly 8% to 9% increases that were common in earlier years.
Still, this year’s average growth exceeded inflation, which slowed to 3.1% in January.
Novo Nordisk raised the list price of Ozempic by 3.5% to $969 for a four-week supply. The company told CNN it raises the list prices of some drugs every year based on changes in the health care system, inflation and market conditions. It noted that the annual price increase of its drugs has not increased by more than a single-digit percentage since 2016.
Eli Lilly last month raised the list price of Monjaro by 4.5% to $1,069 for a four-week supply.
Neither company raised the list prices of drugs approved by the Food and Drug Administration (FDA) to treat obesity. The cost for a four-week supply of Novo Nordisk’s Wegovi is $1,349. Eli Lilly’s Zepbound, which was approved in November, costs $1,060.
For most Americans, the price they pay for drugs depends on their health insurance policies, not on drug manufacturers’ list prices. However, if they don’t have insurance or haven’t met their annual deductible yet, they may have to pay list price.
Many drug manufacturers also offer savings cards and patient assistance programs that can reduce out-of-pocket costs for some people. For example, patients with commercial insurance covering Wegovi and Ozempic can pay as little as $0 and $25, respectively, with the Novo Nordisk Savings Card. People whose commercial insurance doesn’t cover obesity medications can get $500 off the full price of Wegovi.
Eli Lilly offers similar savings programs for Monjaro and Zepbound, providing a 3-month supply for as little as $25 for those with commercial insurance that covers the drug.
While employers and commercial insurers are more likely to cover GLP-1 drugs like Ozempic and Monzaro when prescribed to treat diabetes, many do not cover these drugs for weight loss. Neither do Medicare nor most state Medicaid programs. Additionally, according to Novo Nordisk, people enrolled in government plans do not qualify for the savings card, although some Medicare beneficiaries may qualify for patient assistance that Ozempic will provide at no charge.
Eli Lilly told CNN that it is working with lawmakers to pursue public policy that would expand coverage of anti-obesity drugs by government insurance programs.
Spotty insurance coverage for weight-loss drugs means some Americans must pay out-of-pocket for high-demand drugs, leaving them exposed to rising list prices.
Difficult decisions for patients
The high cost of prescription drugs in general has long been one of the biggest health care problems for Americans. Even those who have health insurance that covers the medications they need may have difficulty paying the cost out of pocket.
The costs of many of the medications Marlene Foss takes forced her to make some difficult decisions last year.
Foss, 72, was taking Entresto for heart failure, which costs $185 a month; And Farxiga, to prevent kidney failure, costs $145 a month in your Medicare prescription drug plan. She decided to stop Entresto because she felt it was not helping her and she did not want to take higher doses, which would have cost even more.
“I had to make a decision,” said Foss, a registered nurse who still works a few days a week to help pay for her medications. “I decided to save my kidney.”

Marlene Foss would rather travel to places like Portugal than spend her savings on medicine. (Courtesy of Marlene Foss)
The Doylestown, Pennsylvania, resident also opted to have a device implanted in her heart last year so she could stop taking the stroke-preventing blood-thinning drug Eliquis because she wanted to free herself from a monthly bill of more than $500. Was. Three years of treatment. Medicare and its supplemental Medigap policy covered the estimated $100,000 cost of the procedure.
Foss has other plans for the money he has saved by “working very hard, on his feet, for 50 years.” She loves traveling and has planned a trip to Italy in May.
“I don’t want to spend all my money on medicine,” he said. “I want to be able to enjoy my life.”
When Mark Rapp signed up for Medicare Advantage in 2020, he was surprised to learn that the medication he takes to manage the permanent side effects of gallbladder surgery would cost $150 a month, which is part of the Medicare Advantage policy. That’s three times more than its cost. former employer.
“I was ready to say, ‘Forget it,'” said Rapp, 68, a former school psychologist who lives in Mansfield, Ohio. “And then I thought, ‘You’re trapped. You have no other choice. You have to take this drug.'”
At first, he tried taking Welchol, which keeps him from getting severe diarrhea every time he eats or drinks, and took only a third of the recommended amount. But this did not help, so he was forced to take the full dose again.

Mark Rapp’s retirement plans changed when he learned how much he would have to pay for prescription drugs if he joined Medicare Advantage. (Courtesy of Mark Rapp)
Although Rapp was able to switch to a $90 generic version of the drug last year, she still has to work full-time as a substitute teacher to help cover expenses. It wasn’t what she planned when she moved from Idaho to Ohio to be closer to her son and grandchildren.
“You can certainly find something else to do with that $90 a month, like putting it in a savings account for grandchildren or using it for travel or shopping,” Rapp said. “That’s an amount I wouldn’t want to pay.”
in political headlines
Lowering drug costs has been one of President Joe Biden’s top talking points in the 2024 presidential campaign as he looks to highlight ways to support consumers.
He often cites the $35 limit on monthly insulin bills for Medicare enrollees, one of several drug-pricing provisions in the Inflation Reduction Act, which Democrats pushed through Congress in 2022.
One of the most notable efforts of his administration is to allow Medicare to negotiate prices for certain drugs for the first time, which is expected to reduce costs for the federal government. Additionally, drug companies are required to pay rebates to Medicare if they raise the prices of certain drugs faster than inflation, which can reduce out-of-pocket costs for some beneficiaries. Both measures were included in the inflation reduction law.
Former President Donald Trump, who is running for re-election, also unveiled several proposals and issued executive orders aimed at reducing drug costs during his administration. He criticized pharmaceutical companies for rising prices.
Some drugmakers have reduced their annual price increases for some drugs amid increasing scrutiny from the White House, Congress and patient advocacy groups. Another factor is recent policies that penalize drug manufacturers for raising list prices faster than inflation.
“We’ve seen the emphasis on growth diminish over time,” said Antonio Ciaccia, CEO of 46Brooklyn. “At the same time, we have seen a greater emphasis on higher starting prices for products.”
(tagstotranslate)medicines
Source link