In efforts to optimize the treatment of primary cholangitis, chronic liver disease New studies have emerged, led by researchers Chris V. Caudle and Gideon M. Hirshfield, affecting the bile ducts. Liver Institute Northwest From Seattle USA and Toronto Center for Liver Disease In Canada, respectively. These support the use of elafibranor And celladelperK agonist Peroxisome proliferator-activated receptors ,PPARFor its short form in English), as an alternative medicine.
It is an autoimmune disease in which the portal tract becomes inflamed and dies. Biliary epithelial cells (cholangiocytes) In small bile ducts. It is caused by genetic, epigenetic, and environmental factors (Figure 1). During its progression, the number of bile ducts decreases, leading to cholestasisis a major factor for the development of fibrosis And cirrhosis, Most patients are between 40 and 60 years of age and the incidence is higher in women. Clinical symptoms include fatigue, itching, etc. progressive jaundice,
Given its slow progression and low prevalence, designing statistically supported trials and evaluating clinical events is a challenge. Biochemical serum markers are currently used as endpoints. level of alkaline phosphatase And bilirubin Can predict outcomes: liver transplant Or death.
He ursodeoxycholic acid It is the first-line therapy, it slows down the biochemical processes and progression. However, 30–40% of patients do not respond, therefore, availability of second-line therapy is important. He obeticholic acid, a bile acid analog, has been approved as an alternative treatment. However, its use is not permitted in people decompensated cirrhosis And itching is considered a possible side effect.
PPARs are members of the nuclear receptor family of ligand-activated transcription factors and include PPAR-α, PPAR-δ, and PPAR-γ. Upon ligand binding, they form heterodimers with the retinoid X receptor and induce transcription of genes involved in inflammation and fatty acid and glucose metabolism. They can also repress transcription of inflammatory genes (Figure 1). PPAR-α is expressed mainly hepatocytes, whereas PPAR-δ has ubiquitous expression, including hepatocytes, macrophages (Kupffer cells), stellate cells, and cholangiocytes. PPAR agonists have emerged as potential treatments for primary biliary cholangitis and other cholestatic liver disorder,
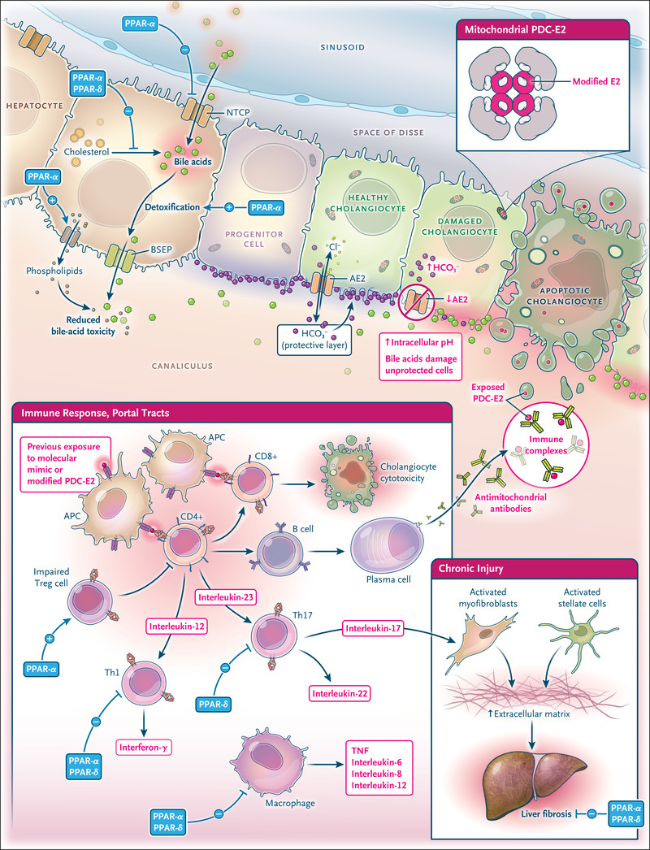
Figure 1: Pathogenesis of primary biliary cholangitis and targets of peroxisome proliferator-activated receptor (PPAR) agonists.
Elafibranor is a dual agonist of PPAR-α and PPAR-δ, and celadelpar is a selective agonist of PPAR-δ (Figure 1). is a major mechanism for both suppression of bile acid synthesis, PPAR-α agonism is known to reduce bile acid toxicity and bile acid absorption by hepatocytes (Figure 1). These remarkable anticholestatic properties are important for the effectiveness of these drugs. Trials with elafibranor and celadelpar resulted in improvements in lipid profiles, which may be mediated by their known induction Fibroblast growth factor 21 (FGF21), Although PPAR-α reduced pain liver fibrosis In preclinical models, only celadelpar reduced liver stiffness and fibrosis in patients with chronic disease.
Although primary cholangitis is autoimmune, immunomodulatory drugs have not shown clinical benefit. PPAR-α and PPAR-δ agonists have anti-inflammatory properties and influence both innate and adaptive immunity by switching macrophages to an anti-inflammatory phenotype and suppressing type 1 helper T cell polarization. PPAR-agonism α induces regulatory T cells. differentiation, whereas PPAR-δ agonism suppresses type 17 helper T cell polarization (Figure 1). It is unknown to what extent these anti-inflammatory properties contribute to the beneficial effects of each drug, although both reduced total IgM and IgG (markers of immune activation) levels, and celadelpar reduced high-sensitivity C- Reactive protein levels reduced. , An important aspect for patients is that Seladelpar effectively relieved itch, the molecular mechanism is still unknown.
Although ursodeoxycholic acid will remain first-line therapy, drug options are increasing for patients who do not respond. People at high risk of disease progression may benefit from early combination therapy. Additionally, people with pre-existing liver fibrosis face a higher risk of inadequate response even with the combined regimen. In such cases, introduction of a antifibrotic drug This can not only delay the progression of the pathology but also potentially reverse existing fibrosis.